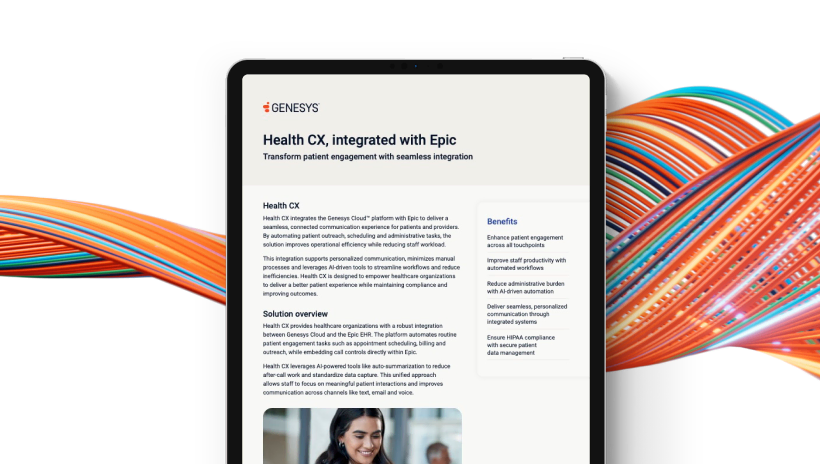
Deliver proactive member engagement that boosts satisfaction and improves quality ratings. Use predictive routing and AI-powered automation to identify interactions that affect ratings and surface content on benefits, claims and care coordination.
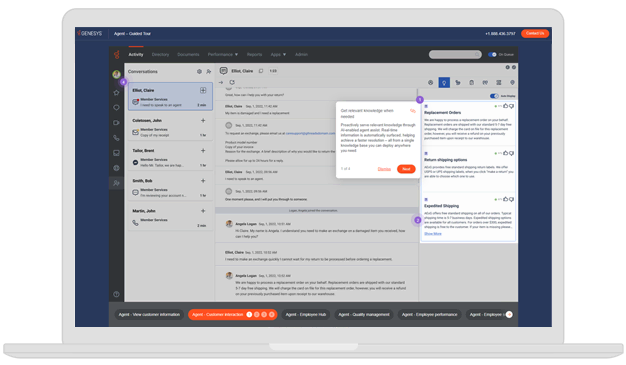
Genesys leads the industry with nine of the top 10 healthcare companies.* Predictive routing quickly connects members to the right resource for improved average handle time, response times and quality ratings. Equip staff with real-time knowledge to provide accurate answers and streamlined service.
Genesys integrates with Salesforce, ServiceNow and other health plan management systems, uniting the patient interaction and communications data with your member data for actionable insights. Proactively reaching out on complex issues, such as denials and prior authorizations, in these systems can prevent inbound activity, drive quality measures and provide the member with information required to resolve their need.
*Based on reported revenue for the respective companies’ fiscal years ended on or before January 31, 2024.