Capture the full cost of risk adjustment with engagement data
Risk adjustment drives how the Centers for Medicare & Medicaid Services pays Medicare Advantage plans, but claims history alone often misses what matters. Health spending isn’t evenly distributed — a small portion of people account for a very large share of total costs. While it’s common to focus on averages, the reality is that few individuals fall near the “average” level of spending. Instead, people’s health status and care needs shift dramatically over their lifetimes, which makes early prediction challenging. This white paper explains why relying only on systems of record, like claims history, overlooks the true effort and cost of serving members.
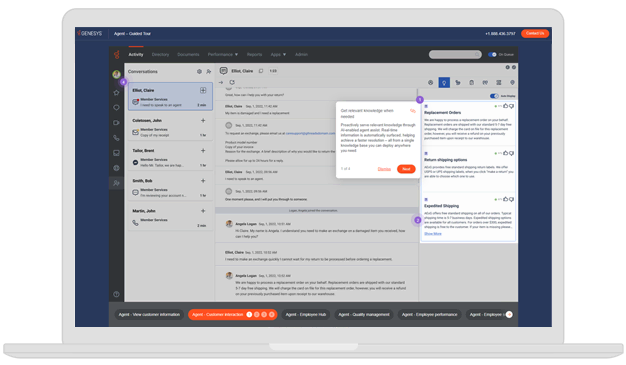
Use your system of engagement — calls, messages, emails and more — to fill that gap. Learn how to combine interaction data with claims to spot rising risk, guide members with the right support and reflect the full cost to serve in plan pricing and reimbursement.