Your Genesys Blog Subscription has been confirmed!
Please add genesys@email.genesys.com to your safe sender list to ensure you receive the weekly blog notifications.
Subscribe to our free newsletter and get blog updates in your inbox
Don't Show This Again.

Most companies recognize that focusing on the consumer experience is the primary way to grow their business and increase loyalty. This is especially true in healthcare, where organizations understand the importance of consumer engagement.
Today, more individuals are choosing their own health plans – and they expect consumer-friendly member service. In addition, patients increasingly demand convenient care options from providers.
Many healthcare entities see customer experience as a priority, but struggle knowing where to begin or which areas focus on to see the most improvements and benefits. Making quick changes in these often siloed and complex organizations only compounds the struggle.
In addition, consumer experience isn’t a singular project. It’s an ongoing discipline that involves a relentless focus on reducing effort — easing friction and making content simple to understand. Offering a great consumer experience means anticipating patient and member needs and offering proactive guidance. It’s about providing compelling, user-friendly self-service. And, ultimately, it means eliminating a member or patient’s need to reach out to the organization for assistance or ensuring they get to the right resources — the first time — to reach a resolution.
Reducing effort requires CX leaders in healthcare to be sure everyone in the organization is aligned and doing their parts toward that goal. Doing so cultivates loyalty. Historically, consumers who have seamless, low-effort interactions with an organization tend to repurchase at a higher rate.
To assess and monitor effort, CX leaders in healthcare can use operational data from the contact center and other areas. These metrics offer an objective view into where consumers are expending effort — and where you can monitor improvement efforts.
Leading consumer experience organizations are shifting their focus from high level metrics like Net Promoter Score and customer satisfaction scores to focusing on effort metrics that are actionable and demonstrated to have more impact on consumer loyalty and retention.
While improving the patient experience in healthcare is a major priority, it’s not the only one. Many healthcare organizations today are also highly focused on reducing costs, especially during uncertain economic times.
The good news: Focusing on effort also highlights opportunities to increase operational efficiency and lower costs. Low-effort experiences have fewer repeat interactions, transactions and escalations, as well as less channel switching. And all of that affects the cost to serve.
Healthcare organizations are increasing membership and growing patient populations through an on-going focus on reducing effort. This drives growth by improving the brand experience and reputation as well as lowering costs.
There are a few ways healthcare organizations can reduce efforts for patients and employees. Here are three key strategies.
Establish baseline effort metrics. Contact centers collect mountains of data. With the right tools, healthcare organizations can use that data to find areas to improve the patient experience. To do so, you need to focus on the right metrics:
Use data to go after quick wins. While some patient experience efforts involve major overhauls over time, there are some areas where organizations can typically achieve quick wins without a major investment.
Looking at same-day repeat interactions (calls or chats) can highlight opportunities to improve routing rules, team member skilling (tools and training), and coaching. Other opportunities include reducing transfers by routing interactions to the right team. In addition, empowering the front line through policy and process changes can reduce hand offs and improve time to resolution.
Lead with data to set strategic priorities. Data often reveals that entire experience domains are suboptimal. Sometimes, analyzing interaction data reveals there’s a high number of interactions per bill or claim. Or the data might show that repeat calls occur most often for certain types of medical encounter or when interacting with specific departments. By using journey analytics and effort dashboards with heat maps, you can identify adverse trends and where consumers are expending increasingly more effort.
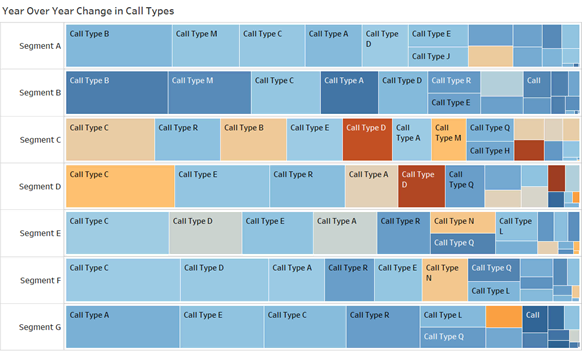
In the example above, we see that “Call type D” is increasing for customer segments D and C. To understand why this is happening, a random selection of calls matching these criteria should be fed through a voice analytics engine that can summarize the topics covered on these calls. It could also be helpful to speak with frontline team members and/or pull call recordings.
Once you have a deeper understanding, you can take corrective action to reverse the trend and improve member and patient experiences.
As you proceed with your analysis, you’ll find plenty of opportunities to reduce patient effort and improve the overall experience. The key is to prioritize these opportunities appropriately, so you focus limited resources on improving the high-impact experiences.
As you create focus areas, communicate your strategy with impacted leaders and across the entire enterprise — from leadership roles down to individual performers — to gain cross-functional alignment on priorities. Key strategic decision points include things like:
Healthcare organizations can use contact center data combined with other operational data to analyze and illuminate where members and patients are expending the most effort. Genesys and AppFoundry® partners provide robust analytics capabilities you can use to identify key improvement opportunities and overhaul your CX strategy.
Remember: CX isn’t a one-time project or series; it’s the discipline of reducing patient effort long-term.
In future blogs I’ll explore how to organize and govern CX work and how to accelerate cultural change in your healthcare organization.
Subscribe to our free newsletter and get blog updates in your inbox.