A post-pandemic Medicaid landscape
The unwinding of pandemic-era continuous coverage protections has pushed Medicaid into one of the most turbulent eligibility cycles in its history. For years, enrollees didn’t have to reverify their eligibility. Now, redetermination requirements have returned — with some states requiring members to reverify eligibility every six months instead of annually — and the effects are reverberating through every part of the system.
For Medicaid Managed-Care Organizations (MCOs), this is no mere administrative shift. It is a structural shock that affects operations, member experience and financial performance all at once.
Coverage churn is rising, eligibility rules are shifting and the people most at risk of losing coverage are often those with the least capacity to navigate complex, deadline-driven paperwork.
In this environment, using the power of artificial intelligence (AI) to help drive member engagement becomes essential. It allows MCOs to understand who is at risk, intervene early and support members who would otherwise fall out of coverage for preventable reasons.
The human reality behind redetermination and churn
On paper, redetermination is straightforward: Verify eligibility, update records and confirm that members still qualify. In practice, it functions as a filter that could disproportionately affect vulnerable groups. Many Medicaid members live below the poverty line, move frequently or lack stable housing. A renewal notice sent twice a year presumes a level of stability that simply doesn’t exist for many households.
That’s why procedural terminations — losing coverage due to missed paperwork rather than ineligibility — may represent a significant portion of disenrollments. Members often discover the problem only when attempting to access care. For instance, a diabetic member learns at the pharmacy counter that coverage has lapsed. Or someone visiting urgent care finds they’re no longer eligible. What should have been a routine renewal instantly becomes a crisis.
From an operational standpoint, these crises multiply. Calls spike, service interactions become more complex and administrative costs rise. The MCO is judged on retention, continuity of care and cost management — yet the root cause is an avoidable breakdown in communication.
This makes proactive engagement not just a courtesy, but a necessity.
Why proactive engagement matters more than ever
A reactive posture means the plan waits for trouble. Members call only after something has gone wrong — and typically when they need care the most. By that point, emotion, urgency and risk are all elevated. Agents must resolve eligibility issues while trying to stabilize a situation that could have been prevented.
A proactive approach moves the intervention upstream. When the plan detects that a renewal is coming due, it can reach out long before coverage lapses. Members receive reminders, instructions and — when needed — personalized help to complete the process. The dynamic shifts from crisis management to collaborative support.
The economics reinforce this shift. One timely outbound contact that helps keep a member enrolled is less expensive than the operational and clinical downstream effects of a coverage gap. Proactive engagement helps strengthen retention, protect clinical outcomes and reduce unnecessary administrative burden.
In other words, redetermination is not only an eligibility exercise; it’s a retention strategy.
How AI sharpens outreach and support
Today, AI has the power to expand what is operationally feasible for health plans managing large, diverse Medicaid populations. While the rules of eligibility don’t change, the ability to interpret patterns, prioritize action and personalize engagement evolves substantially.
Understanding member risk and segmentation
The first step is identifying who is most likely to fall through the cracks. AI models can analyze historical renewal behavior, returned mail and contact preferences to determine which members will require higher-touch support. Instead of treating the population as a monolith, the plan can focus its resources where they will have the greatest impact.
Personalizing outreach across channels
Once risks are mapped, AI and data-analytics help determine the best way to reach each member. Some respond consistently to text messages. Others answer phone calls only at particular times of day. Some require multilingual communication or accommodations for hearing impairment. Right-party contact becomes a practical expression of equity: understanding when, where and how each member is most reachable.
Supporting agents in reactive moments
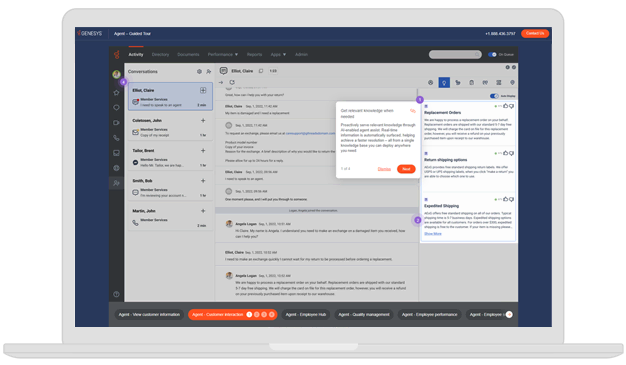
Even with strong proactive engagement, some members will still slip into coverage gaps. AI helps here, too. When a member calls after losing eligibility, the agent can see renewal attempts, prior notices, state rules and potential next steps in a single, streamlined view. Instead of piecing together a fragmented history, the agent can immediately guide the member toward resolution.
Throughout this continuum, AI is not a replacement for human judgment or empathy. It is the mechanism that gives teams the clarity and capacity to intervene earlier and more effectively.
Building a foundation for AI-driven engagement
Of course, designing a successful engagement strategy involves alignment between operational intent, data quality and technology capabilities. AI cannot thrive in isolation from the business processes around it.

Operational coordination across teams
Eligibility specialists, member services, analytics teams, community partners and IT groups all play roles in redetermination. Shared calendars, renewal volume forecasts and clear escalation paths help ensure that outreach is coordinated rather than fragmented. AI-driven signals only matter when teams understand who is responsible for acting on them.
Data and technology readiness
Accurate contact information, language preferences and eligibility data are essential. Every interaction provides an opportunity to refresh or correct these details. Over time, this creates a stronger foundation for predictive outreach and more efficient engagement.
A unified experience orchestration platform ties these elements together — managing outbound communication, capturing conversational history and providing agents with the context they need when reactive help is required.
Equity, language access and cultural sensitivity
Because Medicaid serves many multilingual, low-income and marginalized communities, outreach must respect the lived realities of those members. AI-driven translation can help scale multilingual communication but plans still need oversight to help ensure messages are accessible, culturally relevant and clear.
Privacy and responsible AI
Redetermination outreach deals primarily with administrative rather than clinical information, but privacy remains important. Plans should ensure that models and workflows operate transparently and fairly, especially in determining which members receive more intensive outreach. Responsible AI isn’t a regulatory checkbox — it is part of reinforcing trust in communities that may already feel underserved.
Measuring success and creating a cycle of improvement
The value of AI-driven engagement becomes visible through outcomes, not just outputs. Successful programs evaluate themselves through renewal completion rates, declines in procedural disenrollment, improvements in coverage continuity and reductions in avoidable acute events linked to coverage gaps.
Operational indicators matter as well. When proactive outreach works, inbound call spikes during renewal periods diminish. Member inquiries become more solvable and less highly escalated. Agent experience improves as interactions become more predictable and context-rich.
AI also strengthens the feedback loop. Each outreach sequence generates data about what resonates with members — timing, tone, channel and message structure. Feeding these insights back into risk models and orchestration logic creates a continual refinement cycle. Over time, engagement can become more precise, more equitable and more effective.
Preparing for the future of Medicaid eligibility
Redetermination is not a one-time event tied to the end of pandemic protections. Policy shifts — from more frequent eligibility checks to changing income thresholds and work requirements — are poised to reshape the cadence of Medicaid enrollment for the foreseeable future. That means churn risk is not a temporary anomaly. It is a structural condition that requires long-term strategic planning.
Health plans that use AI-driven engagement solely to manage today’s unwinding period may find themselves repeating the same challenges in the next cycle. Plans that treat redetermination as a catalyst for transformation, however, can build engagement models that scale as rules evolve and member needs change.
This perspective reframes redetermination as a recurring opportunity: a chance to strengthen trust, stabilize membership and improve outcomes for those who rely on Medicaid the most.
Turning administrative burden into member connection
The process of Medicaid redetermination will always carry risk — for members, for care continuity and for plan operations. But with targeted, AI-powered outreach and modern experience orchestration, health plans can shift from reacting to lapses to actively preventing them, avoiding unnecessary friction for everyone involved.
Most importantly, that shift delivers more than operational efficiency. It supports healthier communities, strengthens equity, reduces avoidable crises and stabilizes the member base that MCOs are entrusted to serve.
In a landscape where coverage can be fragile, helping eligible members stay connected to care is one of the most meaningful ways a health plan can demonstrate its value. AI-driven engagement gives plans the tools to do exactly that — consistently, proactively and at scale.